
Contrary to some beliefs, the Affordable Care Act is still in place today. It continues to provide more than 30 million Americans with healthcare coverage.
Even though Congress has modified the original law, it still has compliance requirements attached to it. Understanding these requirements will ensure your business doesn't incur financial penalties.
This article will tell you all you need to know about ACA reporting deadlines and what to do if you miss them.
The Affordable Care Act
Congress enacted a comprehensive healthcare reform law called The Affordable Care Act (ACA) in early 2010. It's also known as PPACA and Obamacare. There are three main targets for the law.
- The first is to give more Americans access to affordable health insurance. The government gives consumers a subsidy called the premium tax credit. The credit lowers the costs of health insurance.
- The second is to expand Medicaid. Medicaid should cover all American adults below a specific threshold of the federal poverty level (FPL). However, thus far, not all states have expanded their Medicaid programs.
- The last is to support new medical care practices and methods. In theory, advanced innovations should lower the costs of healthcare for all Americans.
What is ACA Reporting?
The Affordable Care Act requires employers with more than 50 full-time employees to file federal ACA documentation annually. The government calls these companies Applicable Large Employers (ALEs). It also requires businesses of any size with all self-insured employers to file.
Each year, your company has to determine its ALE status. The IRS uses the information about healthcare coverage provided to full-time employees to give out tax credits. They also use it to organize employer shared responsibility provisions.
ACA Reporting Requirements
The IRS released draft versions for 2021 forms. Providers of minimum essential coverage (MEC) need to use forms 1094-B and 1095-B. Self-insured plan sponsors that aren't ALEs also need to use these forms. These forms report under section 6055.
All ALEs use forms 1094-C and 1095-C under Section 6056. In addition, combined Section 6055 and 6056 reporting by ALEs sponsoring self-insured plans need to use these forms.
Companies need to submit filing copies to the IRS and all employees. Furthermore, there are state-based compliance requirements you will need to submit.
However, the IRS hasn't released instructions for the draft forms yet. Therefore, the IRS can still make changes to the documents before releasing them. But, significant changes are unlikely.
Important Dates for Reporting
As the year comes to a close, it's essential to understand the ACA reporting deadlines for 2021. Again, these are draft dates, so you should stay up-to-date with any changes. Here are the most critical filing dates to remember.
You must provide individual statements for 2021 by January 31, 2022.
- If you are filling out paper IRS returns for 2021, you must file them by February 28, 2022.
- You must submit electronic IRS returns for 2021 by March 31, 2022.
- If you have more than 250 1095-C Forms, you may only submit the forms electronically.
- If you need an extension, you can submit Form 8809 for an extra 30-days. However, you must file the form by January 31, 2022.
Financial Penalties
Form 1095-C provides employee enrollment details, so failure to provide them to your employees on time can result in penalties.
Let's look at the steep financial fines you need to be aware of when compiling your ACA reporting documentation.
If you fail to submit ACA information returns within 30 days after the deadline, you could be subject to a $50 fee per return (employee) not filed. The penalty will not exceed an annual maximum of $556,500.
After 30 days, the penalty increases until August 1, 2022. Until August 1, the fee goes to $110 per return not filed. The liability will not exceed an annual maximum of $1,669,500.
After August 1, the fine increases again to $270 per return. The annual maximum will not exceed $3,339,000.
There's also a general fine of $280 for late or incorrect 1095-C Forms given to employees. But, then, there's an additional $280 fine for late or inaccurate 1094-C Forms and copies of 1095-C Forms filed with the IRS.
This means the IRS may fine you $560 per employee. But, the annual maximum will not exceed $3,426,000.
Unfortunately, if you, as the employer, willfully miss the deadline, the penalty is $560 per turn. There is no annual maximum limit. Therefore, you may be subject to huge fines.
Thus, even if you missed the deadline for ACA reporting, it's better to file late than not to file at all.
ACA Employer Mandate
ALEs have to pay MEC to at least 95% of their full-time workforce. Also, employers in conjunction with Employer Shared Responsibility Payment need to do so. Employer Shared Responsibility Payment is the ACA's Employer Mandate.
Those who fail to do so may incur additional fines under IRS Letter 226J.
The 2021 penalty was $2,700 per year, per employee, minus 30.
Important Notice
The IRS hasn't finalized fees for the 2021 reporting year, so they are subject to change. Again, it is your responsibility to confirm with the IRS the exact dates as filing time approaches.
Benefits of Using an ACA Reporting Service
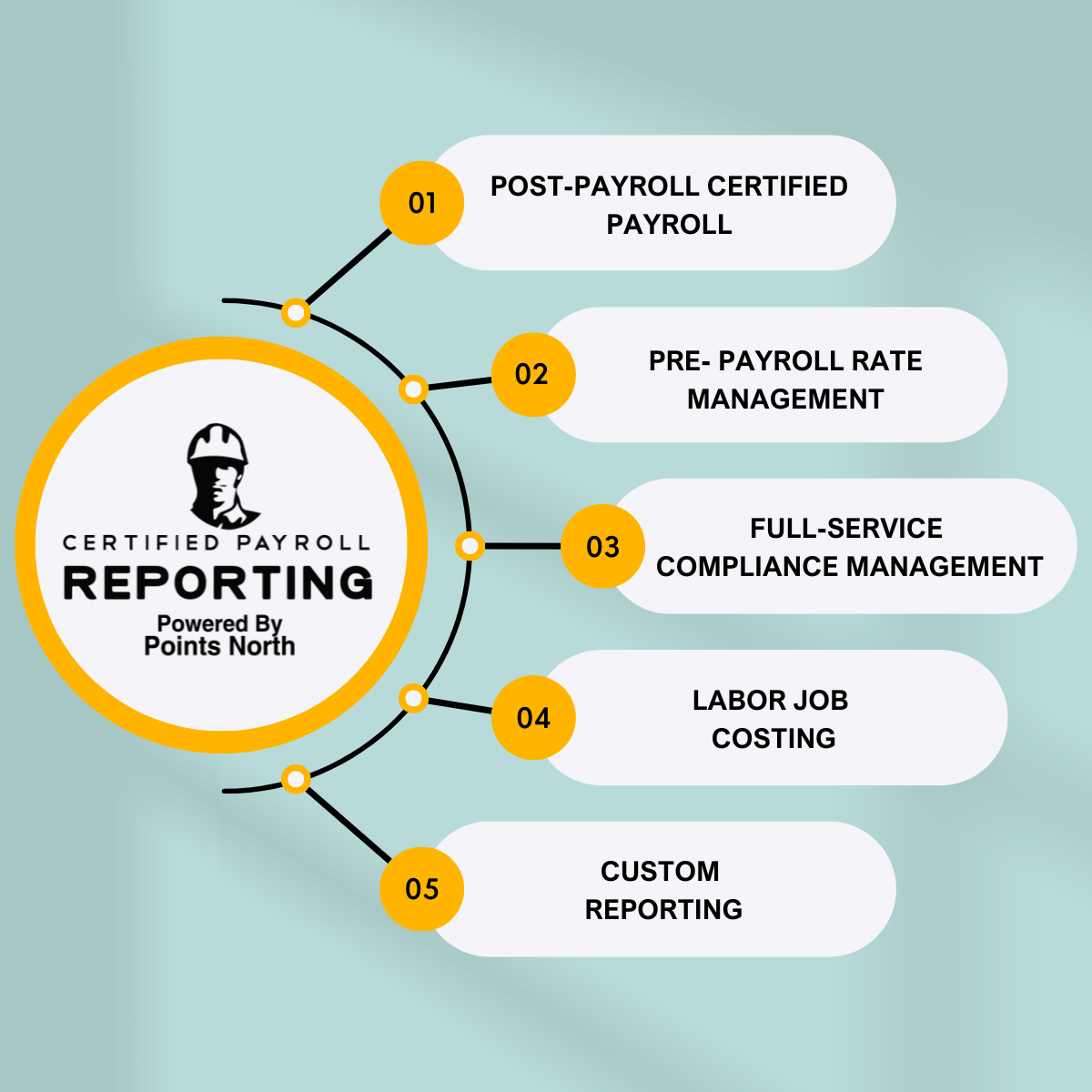
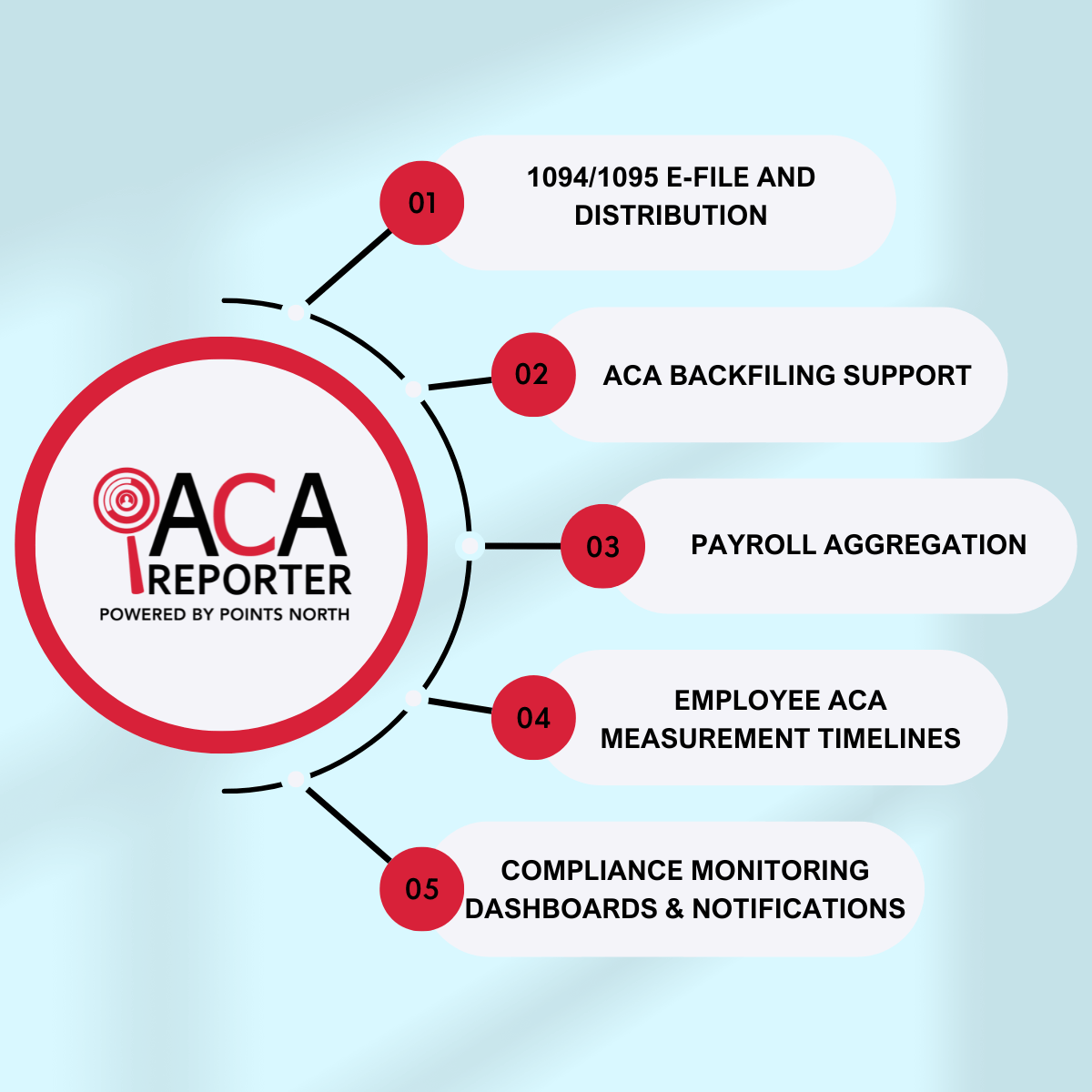
Accurate IRS ACA reporting means staying up-to-date with regulatory requirements and policy changes. You also must navigate employee data to ensure you fill out all the forms correctly. It's a full-time job. Thus, it would help if you considered working with an ACA reporting service.
A reporting service tracks all the rules and regulations in real-time, so you never have to worry about changing paperwork and employee data.
Most importantly, your service provider will not only file your forms correctly but also on time. This means you will avoid all the hefty penalties imposed by the IRS.
Prepare Your 2021 ACA Reporting Today
With less than three months left in 2021, you must start preparing your forms for ACA Reporting now. With so many forms, deadlines, and fees to worry about, you are best off working with a reporting service.
To get started with your ACA reporting service, contact us at Points North. Our experts are ready to streamline your ACA reporting process and leave you feeling stress-free.



.png)