The IRS has advised that employers, along with their service providers, be prepared to give employees their health care reporting forms in order to ensure a timely submission. Deadline extensions will not be granted for 2022.
The ACA requires Applicable Large Employers (ALEs) to submit reporting forms to the IRS and distribute them to workers.
What Are ALEs?
An Applicable Large Employer is any entity that employs on average at least 50 full-time or full-time equivalent employees during the preceding calendar year. This calculation excludes all employees who work 30 hours or fewer per week, which are generally not counted toward establishing coverage eligibility by ACA standards, and also excludes all employees under age 18 who have not yet graduated from high school because they often have access to family coverage outside of employment. Anyone falling into these categories should consult with a specialist in labor law for relief options before abandoning their job because it does not meet ACA requirements for coverage eligibility.
ACA Deadlines:
- Jan. 31, 2022
- 1095 Forms delivered to employees
- Feb. 28, 2022
- Paper filing with IRS
- March 31, 2022
- Electronic filing with IRS
Over time, the IRS has often prolonged these deadlines, according to legal counsel at Jackson Lewis in Baltimore. "In the past, such extensions were intended to help businesses adapt to the new regulations. Most recently, a further extension was announced in Notice 2020-76 for plan year deadlines to account for COVID-19 epidemic difficulties."
On October 2, 2020, the IRS released Notice 2020-76. This delayed the deadline to provide Forms 1095-C and 1095-B from January 31, 2021, to March 31 of the same year. As of yet, there has been no news on a 30-days extension for the 2022 filing.
We may only presume that the deadline for 2022 has not been extended, implying that it will fall on January 31, 2022. This deadline is for employees to receive 1095-B and 1095-C forms. February 28, 2022 is the due date for those who want to submit paper copies, while March 31, 2022 is the due date for those who wish to submit electronically.
The IRS has not yet issued the penalties for late reporting in 2022. Filing with incorrect information, for example, using the wrong codes or TIN, may result in a penalty. You may also be fined if you submit late without providing an acceptable excuse, or if you file with the incorrect medium.
"No such extension has been announced (nor is expected) for reporting in the first quarter of 2022," Thomas wrote. This implies that employers subject to the ACA's reporting provisions should work internally or with their extraneous suppliers to meet these dates.
"Employers should not expect any extensions and should work hard to complete their reporting forms on time," says Danielle Capilla, Vice President of Compliance, Employee Benefits at Alera Group, a network of insurance and financial services businesses.
Employers often prefer to distribute 1095 forms to workers along with their W-2 tax forms, as both are due on Jan. 31, according to Ms. Vassiliadis.
ACA Reporting Forms
The IRS has released final versions of ACA forms for reporting on plan year 2021 coverage.
Transmittal Forms:
1094-B- For filing Forms 1095-B to the IRS.
1094-C- For filing Forms 1095-C to the IRS.
Reporting Forms:
1095-B- Used by insurers and small, self-funded employers to provide exact enrollment information of employees and family members enrolled in minimum essential coverage.
1095-C- Used by ALEs, whether fully insured or self-funded, to detail their offer of coverage so as to avoid potential employer mandate penalties. For each full-time employee, a 1095-C must be provided to them and submitted to the IRS upon completion. Self-insured ALEs must also file a Form 1095-C for any part-time employees who are enrolled in coverage.
ACA Requirements:
employer fines levied against ALEs that do not provide required coverage to full-time employees under the statute's shared responsibility provisions are still in effect. By submitting forms with the IRS and providing copies to workers, ALEs demonstrate they offered eligible staff health insurance that complied with the ACA.
Employers with 50 or more full-time workers must provide coverage to all their employees that meet the required levels of affordability and minimum value. They are subject to penalties if they do not comply. Employers with less than 50 full-time workers are not obligated to offer health insurance, but if they wish to do so, it must fulfill ACA requirements
Self-insurers:
All of the information required by the Affordable Care Act for ALEs is collected in the Form 1095-C, and individuals who are not covered will not be sent a Form 1095-B.
Smaller organizations (non-ALEs) that sponsor self-insured plans:
They are not required to furnish Form 1095-B to covered individuals, but they are required to send them a 1095-C if they comply with certain conditions.
Penalties
The IRS has the right to penalize your company for failing to file your ACA forms on time. The IRS may subject a company to a penalty payment if they submit incorrect or late forms. For failing to provide correct 1095-C or 1095-B forms to an employee, the IRS can fine up to $280 per form. A separate $280 per form penalty may be imposed for each missing form filed with the IRS, resulting in a potential $560 per employee penalty.
The above penalties are for incorrect reporting and are separate from ACA penalties for inadequate coverage:
- ALEs that fail to offer minimum essential coverage to at least 95 percent of their full-time employees and dependents are facing a $2,750 penalty per employee, or $229.17 per month for the 2022 tax year, under Section 4980H(a). The determined amount will reduce 30 full-time employees from the total number of full-time employees.
- The Section 4980H(b) penalty, which is assessed for each employee who receives a premium tax credit/subsidy from a state or federal ACA marketplace exchange when the ALE does not provide a coverage option that meets the affordability threshold, is anticipated to be $4,120 per person or $343.33 per month for the 2022 tax year.
The IRS sends Letter 226-J to notify ALEs that they may be required to pay an employer shared responsibility payment.
The Bottom-Line
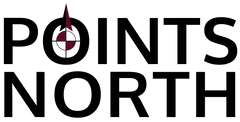
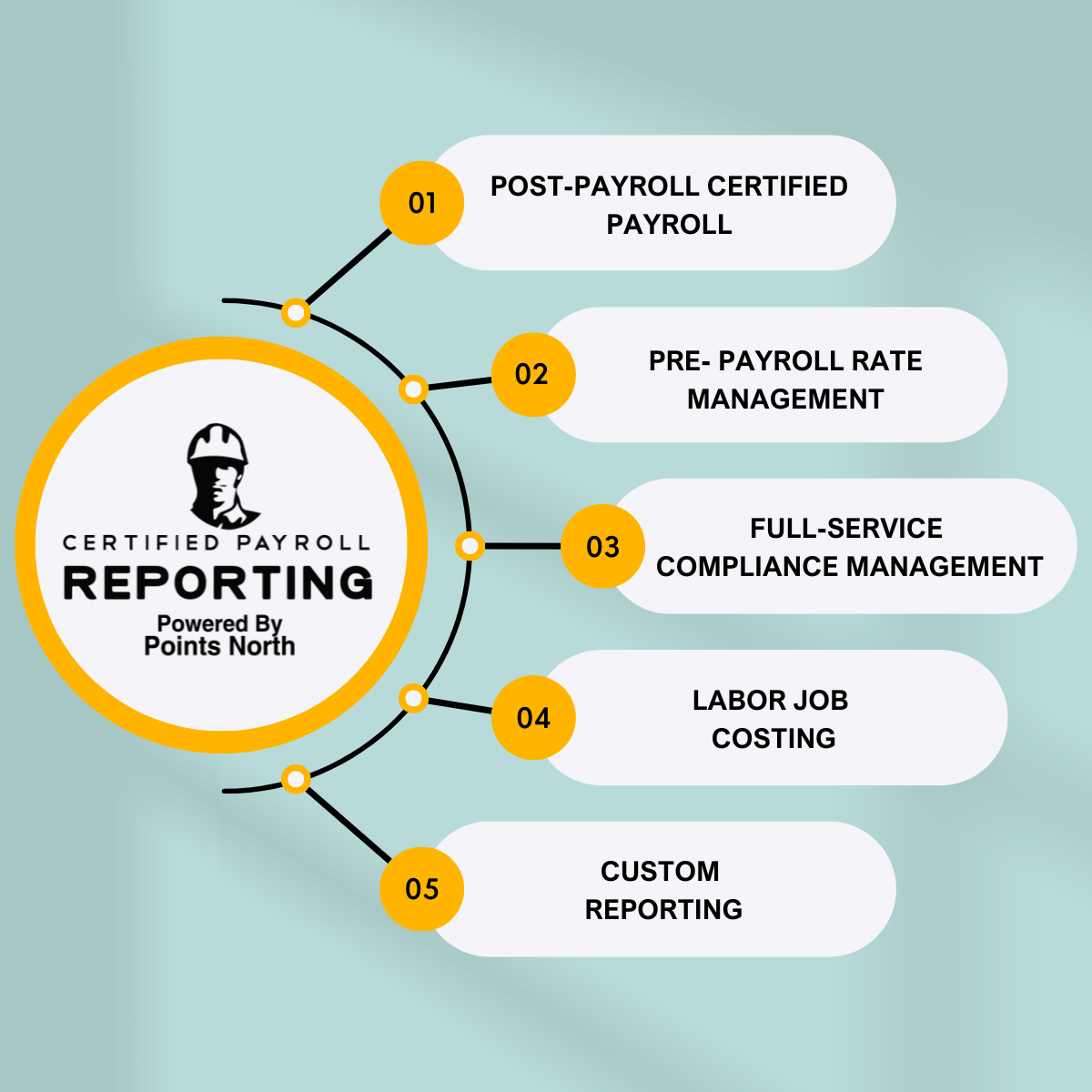
In conclusion, the Affordable Care Act (ACA) requires Applicable Large Employers to submit reporting forms and distribute them to their employees. The IRS will not extend any deadlines for 2022 when it comes to ACA reporting requirements. This means that employers should make sure their employees are ready for 2022 in order to avoid penalties from the IRS. Contact us today to help streamline your ACA reporting and keep your company in complete compliance!



.png)