Maine, New Mexico, and Kentucky have successfully moved away from the federal Healthcare.gov marketplace and launched their own state-run Healthcare marketplace on October 4. These three states join 14 other states and the District of Columbia whose exchanges will be operated by their state's government, which leaves only eight state-run "partnerships" with the federal government.
Publicly operated health insurance marketplaces will provide coverage to more than 1.2 million people who would otherwise purchase their plans through Healthcare.gov.
Maine
Maine's new coverme.gov website will help implement the ACA marketplace. “The state has more control and will be better able to customize outreach efforts,” said Maine-based independent health insurance advisor, Mitchell Stein.
"However, if everything goes as planned, the website should be extremely transparent to the end user, but they will be purchasing the same plans.
New Mexico
New Mexico, like Maine, has an entirely new marketplace website: bewellnm.com. The exchange offers a number of tools to assist state residents in obtaining low-cost medical care. According to a news report from healthinsurance.org, the new state-based exchange will feature five insurers' plans, which is more variety than most of the United States.
Kentucky
Kentucky's road to a state-run exchange is more winding than Maine's and New Mexico's. Kentucky Governor Andy Beshear has reactivated the kynect.ky.gov platform, which was first launched in 2017 by his father and former governor, Steve Beshear.
According to the Richmond Register, the platform will serve as a one-stop shop for Kentucky residents applying for Medicaid and “other resources, including Supplemental Nutrition Assistance Program (formerly known as food stamps) and family and child-care assistance programs.”
Residents of Kentucky will be able to purchase Anthem health plans in every county. For the first time, residents will have the option to buy vision insurance through their state-run ACA health exchange.
The States Stand
Health and Human Services Secretary (HHS), Xavier Becerra, praised the three states' transition to a state-based ACA health exchange, noting that "hundreds of thousands" of people in Kentucky, Maine, and New Mexico now have alternative coverage options that may be tailored through the State-based Marketplace. "The Biden-Harris Administration is committed to assisting states in their efforts to ensure that individuals have good, affordable coverage."
For the 2022 plan year, all three states will use their own exchanges. Enrollment will open on November 1 and run through January 31 of the following year, like it does at the federal level.
Meanwhile, the federal open enrollment is set to be one of the most successful in history. The period will last for 30 days, and there will be considerably more resources available for outreach efforts and educating people about healthcare choices. In addition, insurers are adding to their ranks for the 2022 ACA plan year, which will undoubtedly make coverage more readily accessible.
The recent results of numerous polls reveal that the healthcare law's popularity is increasing among Americans, and for the first time in a long time, the future of the ACA appears bright.
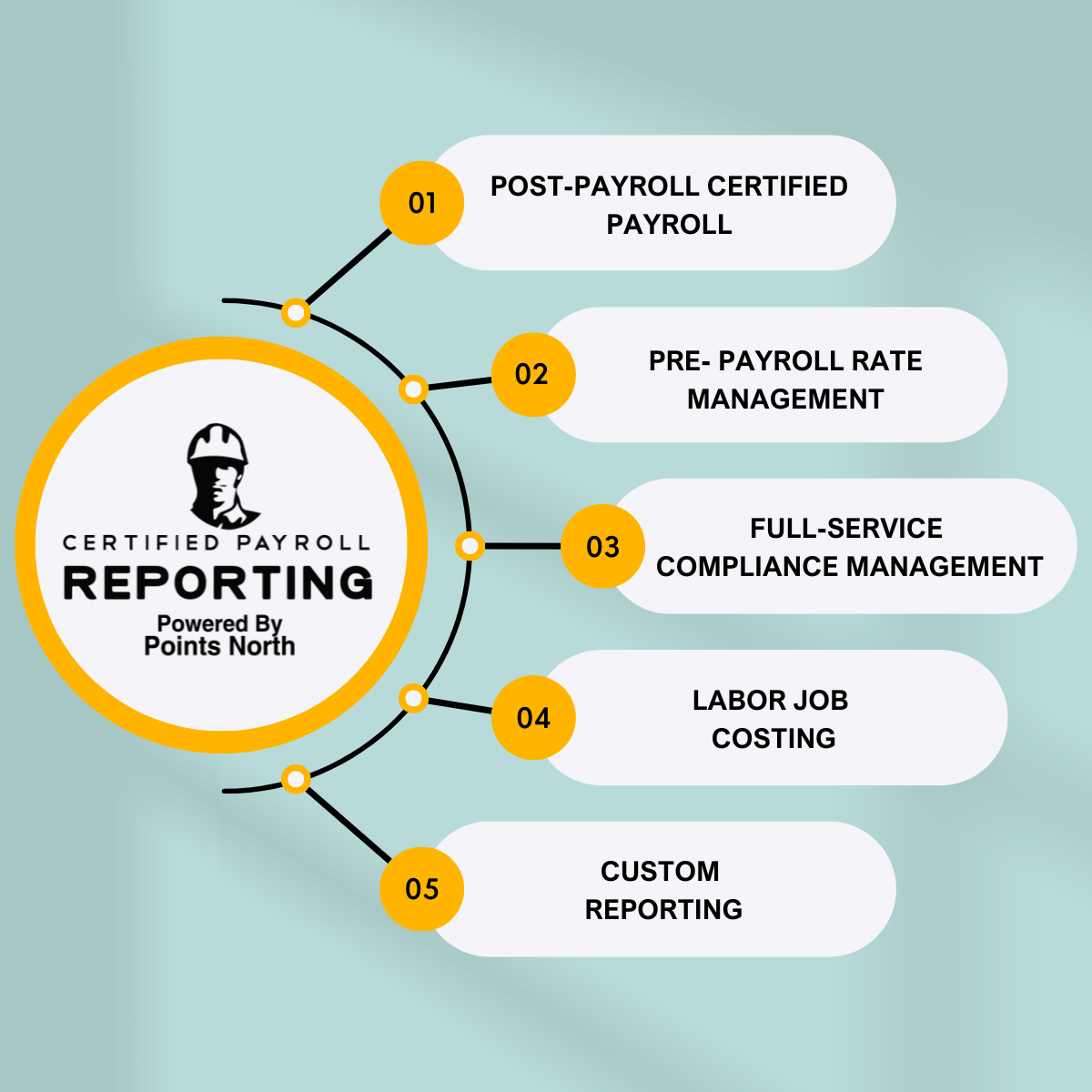
Despite the fact that the Affordable Care Act has become even more popular, employers must be cautious about their ACA Employer Mandate obligations — they're not going anywhere, and in fact, they're becoming more complicated.
Employers with 50 or more full-time workers and full-time equivalent employees are known as Applicable Large Employers (ALEs) under the ACA's Employer Mandate, which requires them to:
- At least 95% of their full-time workers (and their dependents) must be covered by an affordable health insurance policy that meets Minimum Value.
- Verify that the premium is reasonable based on one of the IRS-approved methods for determining affordability.
Organizations that are not taking their ACA Employer Mandate responsibilities seriously should reconsider their stance, as the IRS has recently made clear its intentions for increased enforcement.



.png)