
The IRS said that there is no statute of limitations for ACA penalties. It means that ACA non-compliance penalties can be issued for any reporting year at any time in the future.
It is a significant development that is impacting employers' ACA compliance strategies across the United States. The IRS Office of Chief Counsel issued a field notice.
In the notice, the IRS clarifies that the Employer Shared Responsibility Provisions (ESRP) imposed by IRC Section 4980H are not subject to the statute of limitations.
What is ACA Employer Mandate?
According to the ACA Employer Mandate, Applicable Large Employers (ALEs) are employers with 50 or more full-time employees and full-time equivalent employees.
ALEs must provide Minimum Essential Coverage (MEC) to at least 95% of their full-time employees and their dependents under the ACA Employer Mandate.
Such coverage should meet the Minimum Value (MV) and must be affordable for the employee. Otherwise, you will be subject to Internal Revenue Code (IRC) Section 4980H penalties.
What Are The Employer Shared Responsibility Provisions?
The Employer Shared Responsibility Provisions require ALEs to provide health insurance that:
- Is considered affordable coverage
- Offers the MV to full-time employees and their dependents
- Meets the MEC requirements for covered services and procedures
The plan should at least cover 60% of the total allowed cost of the benefits incurred under the plan. Health insurance should not cost more than about 10% of the household's income. But, the exact percentage of the household's income changes with inflation.
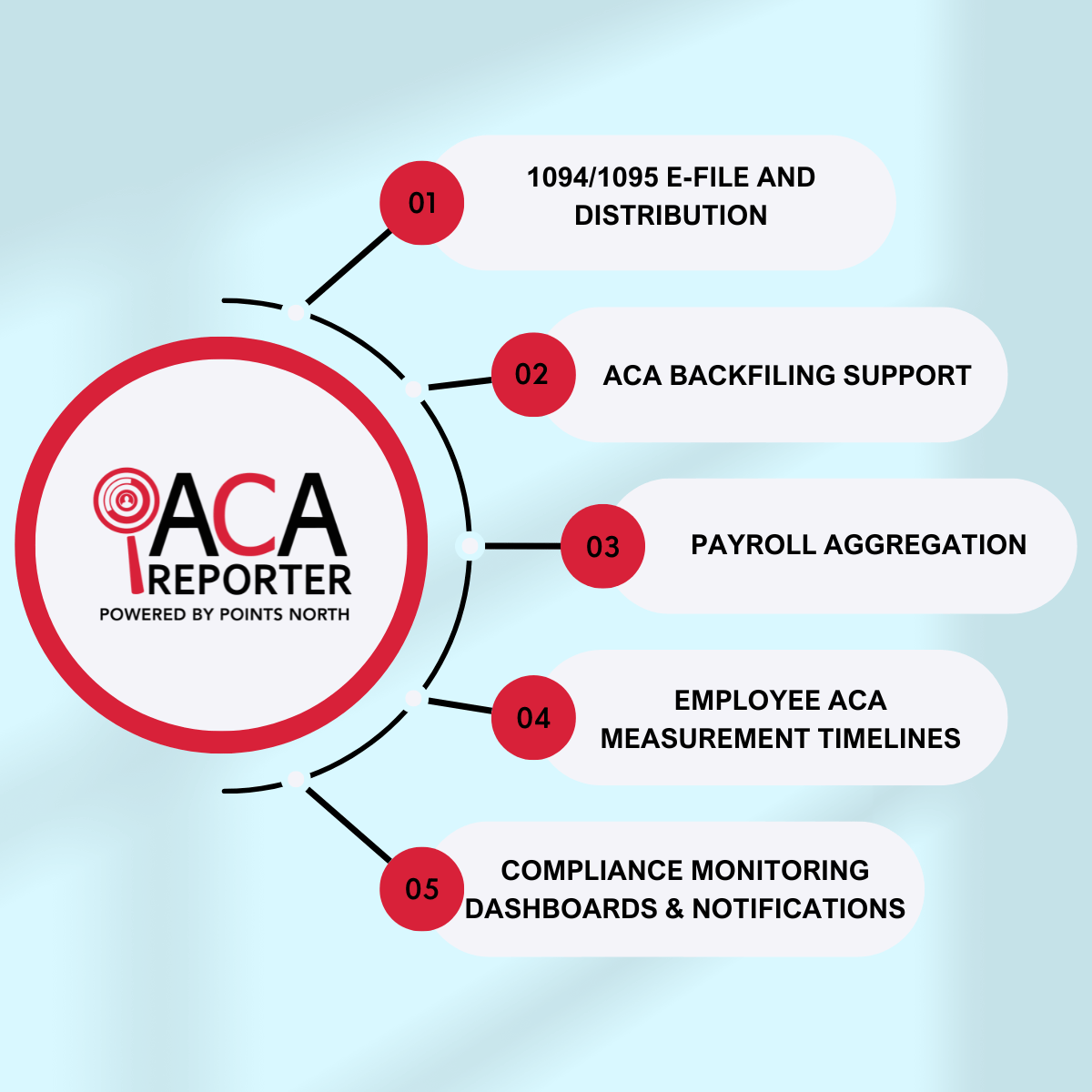
ALEs must also file Form 1095 and Form 1094 to the IRS annually. Form 1095 and Form 1094 document the ACA compliance. Employers will owe the ACA tax penalty payment to the IRS if they fail to:
- File Form 1094 or Form 1095
- Provide affordable healthcare with MEC
Difference Between The IRC Section 4980H(a) Penalty And IRC Section 4980H(b) Penalty
| IRC Section 4980H(b) Penalty | IRC Section 4980H(b) Penalty |
|---|---|
| The IRC Section 4980H(b) penalty may apply if an ALE fails to provide coverage to all full-time employees. It also applies if ALE's coverage is not affordable or doesn't offer minimum value. | The IRC Section 4980H(b) penalty may apply if an ALE fails to provide coverage to all full-time employees. It also applies if ALE's coverage is not affordable or doesn't offer minimum value. |
| The IRC Section 4980H(b) penalty is calculated as $3,000 (as adjusted) x ALE's number of full-time employees that receive an Exchange subsidy. | The IRC Section 4980H(b) penalty is calculated as $3,000 (as adjusted) x ALE's number of full-time employees that receive an Exchange subsidy. |
How Can It Affect Your Business?
Suppose your business did not comply with the ACA Employer Mandate for the 2015 tax year. Generally, the IRS limits a taxpayer's statute of limitations to three years.
It means that the agency has until 2018 to audit your business and issue an ACA penalty assessment. But, since there's no statute of limitations for ACA penalties, the IRS can audit 2015 ACA filings and issue the Letter 226J penalty at any time.
The IRS can use its levy or lien powers against your property or business if your business does not pay an ACA penalty assessment. IRC Section 4980H penalties are issued via Letter 226J to employers who did not comply with the ACA Employer Mandate.
What Does The IRS' Notice Of No Time Limitations For ACA Penalties Mean?
For the 2018 tax year, the IRS is issuing Letter 226J penalty notices. The IRS' notice of no time limitations for ACA penalties means that previous year's ACA non-compliance penalties are fair game. The passing of time will not grant a reprieve for employers who failed to comply with the ACA.
If your business didn't receive an ACA penalty for a prior year and you know that your business didn't file correctly, we suggest you address the issue proactively. ACA Penalty Risk Assessment can help your business identify possible risks in your ACA filings and allow you to make corrections.
ACA Employer Mandate Reporting Requirements
The ACA Employer Mandate reporting requirements were first required in the 2015 tax year. The reporting requirements were met with some concern. Employers were unsure of how diligent the IRS would be in the assessment of non-compliance.
The ACA Employer Mandate reporting requirements are becoming more complex each year because of:
- Increased scrutiny from the IRS
- The introduction of new 1095-C codes
- Individual ACA state reporting requirements
Non-Compliance With The ACA Employer Mandate Reporting Requirements
A lot of developments have happened. It indicates that the IRS is coming for your business if you ignore the reporting requirements and healthcare law compliance. For example, a recent report from the Treasury Inspector General for Tax Administration (TIGTA) found that the IRS calculated more than $15 billion in ESRPs for the 2018 tax year.
It is almost double the amount calculated in the 2015 tax year. But, the total amounts collected from employers who did not comply with the ACA were lower. Therefore, TIGTA has recommended that the IRS do more to:
- Improve the process of identifying non-compliance
- Issue penalties to employers who filed incorrectly
The agency said that 2020 would be the last year for Good-Faith Transition Relief. As a reminder, Good-Faith Transition Relief was extended every year in the past. It provided relief to employers that reported incomplete or inaccurate information on their ACA returns.
For the 2022 fiscal year, President Joe Biden requested additional funding for the agency's tax enforcement efforts to amplify the situation. It will provide the agency with more resources and tools to identify ACA non-compliance. These advancements illustrate the importance of sound ACA compliance processes and correct filings.
The Bottom-line
If you need help with your ACA compliance strategy, contact us to learn more about ACA compliance, reporting requirements, and essential ACA state filing deadlines. If your business is unsure of your prior years' filings, have an ACA Penalty Risk Assessment performed.
It will provide your business with complete visibility into the IRS penalty exposure. It will also allow you to take action before the agency issues a penalty. Since there's no statute of limitations for the ACA penalties, the question you should ask yourself is when the IRS will audit your business.



.png)