
Did you know that 28 million people went without health insurance in 2020? If that sounds like a lot, that’s because it is - that’s almost 1 in 10 people in the US that were uninsured that year.
But what does that mean for you, your business, and your employees? And how does the Affordable Care Act impact that?
Learn more below about the ways the ACA has changed small group coverage over the years and what the future of the ACA may hold!
Affordable Care Act Basics
By now, most people are familiar with the Affordable Care Act, but there are a few aspects of the program that are lesser-known.
The Affordable Care Act, also commonly referred to as the ACA, has three main goals.
The first of these goals is to increase people’s access to health insurance by providing more affordable options for health coverage. The ACA does this by providing tax credits to individuals that assist with the payment of health insurance premiums. Anyone who has an income between 100% and 400% of the Federal Poverty Level (FPL) qualifies for this subsidy.
The second goal is to push for the expansion of Medicaid programs across the country to include any adult whose income is less than 138% FPL. It may come as a surprise to those living in states that have already opted for this expansion, but several states have yet to do so.
The third goal of the ACA is to encourage innovation within the healthcare industry that will allow for lower overall costs of care. One notable change the ACA has provided to the industry is that health insurance providers are no longer able to deny someone coverage or increase someone’s premiums due to pre-existing conditions!
Historical Small Group Trends
Over the last decade of the Affordable Care Act being in place, the trends in small group coverage have stayed mostly the same. In fact, consistently, about half of small businesses have offered health insurance to their employees since 2013.
However, you do begin to see some slight shifts in coverage trends when you start breaking down the “small business” category more.
Per a study completed in 2017, the percentage of small businesses that offered health insurance coverage seemed to increase relative to the number of employees the business had. On average, for companies that reported between 3 and 9 employees, about 50% of them offered employer-sponsored health insurance. Compare that to companies with 10 to 24 employees at 73% and companies with 25 to 49 employees at 87%, and there’s a clear trend here.
But why may that be? It’s not a totally straightforward answer. One key factor that plays into this trend is the affordability of employer-sponsored health coverage. Another key factor is employees of small businesses opting for individual coverage at a lower rate thanks to the previously mentioned tax credits.
However, this coverage trend is a little more complicated than the numbers may make it seem.
Keep reading to learn more about the ways small group coverage continues to change and the barriers that small business owners are facing today.
The Affordable Care Act in 2022
During the last year, several changes to the ACA occurred that will likely bring with them an impact on small group coverage trends.
Individual Coverage
One of the most notable of these changes is the fact that there are more low-cost plans available to individuals than ever before. Across the board, premium costs decreased by an average of 3% in 2022.
Another important change seen in 2022 is an increase in tax credits available for individuals. Anyone making more than 400% FPL used to be unable to benefit from cost-reducing assistance through the ACA. However, new changes to the policy have expanded to cover those above 400% FPL by capping costs of benchmark plans to 8.5% of someone’s income.
On top of these changes, the annual Open Enrollment Period (OEP) for individuals has been lengthened, and more states have joined the federal health insurance marketplace.
Small Group Coverage
Though no data is available for small group coverage rates this year, there are already significant changes to be seen for individual enrollment rates. As of the end of the 2022 OEP, almost 14 million individuals enrolled in healthcare coverage through the ACA marketplace compared to only 11.4 million in 2020.
Alongside these changes to the ACA regarding individual coverage, many small businesses are reporting an increase in healthcare costs due to COVID-19. In fact, a third of small business owners are now reporting that they are struggling to afford coverage for their employees and themselves.
To deal with this lack of affordability in the current economy, many small business owners have had to make the tough decision to decrease their benefits. For those that have made that choice, 1 in 3 have opted to lower their employer contribution to their employee’s health premiums, and roughly 1 in 2 have chosen new plans that offer lower premiums and oftentimes less coverage.
With more access than ever to individual coverage options through the ACA and small businesses struggling to stay afloat, what will this mean for the future?
What to Expect Moving Forward
Nobody can predict the future, but it’s safe to assume a shift in small group coverage trends may be on the horizon.
As small business owners are becoming less able to afford group policies and individuals are seeing ever-increasing incentives to opt for their own coverage, it is possible small group coverage will see a decline.
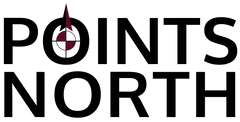
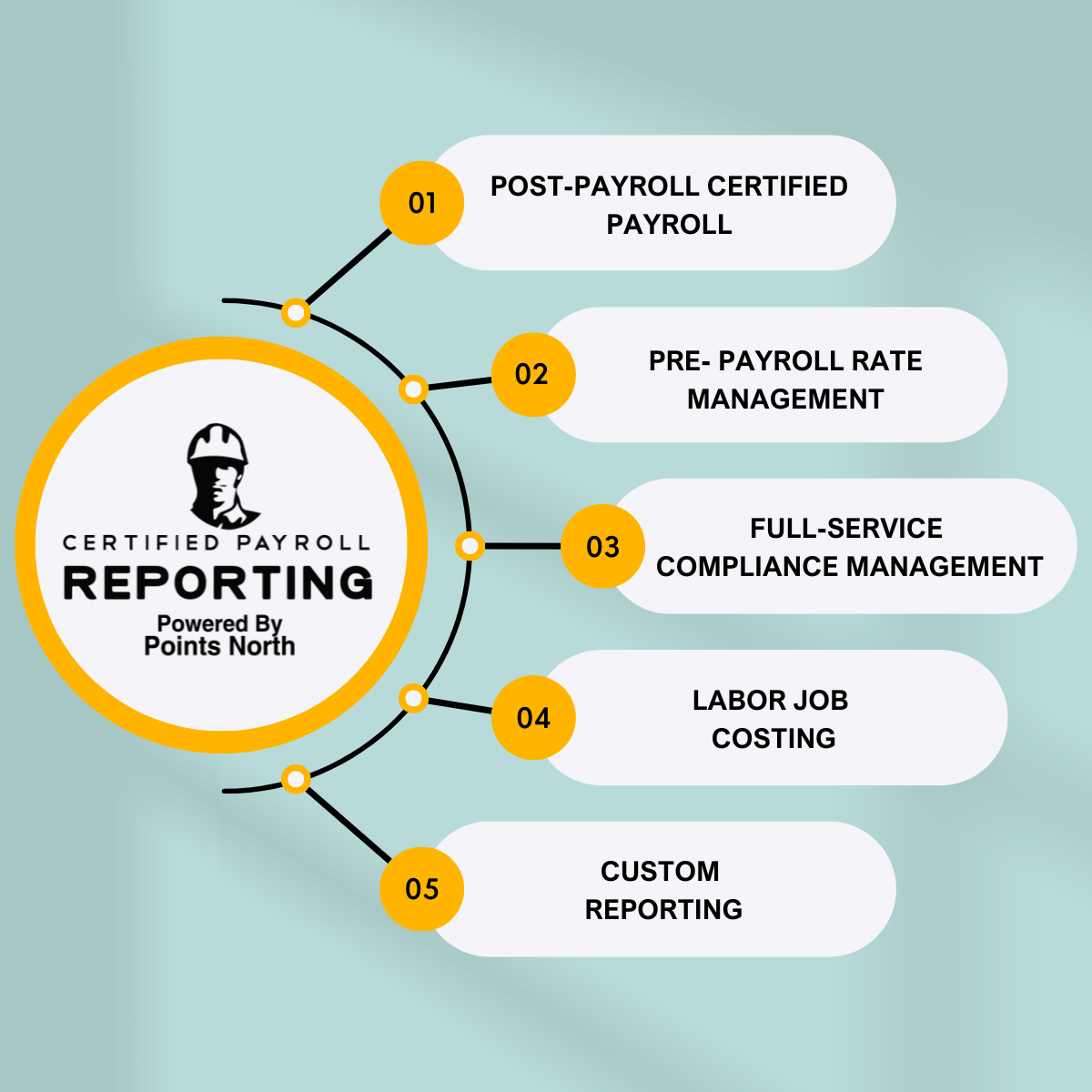
Regardless of what the future may bring, it is important to report ACA information accurately. Give our ACA reporting system a try and let us handle that for you!



.png)