The fourth quarter is just around the corner. With the beginning of the fourth quarter comes the inevitable tax filing season.
Employers should pay close attention to the ACA reporting requirements this year because some significant developments will add complexity to the now seven-year-old reporting requirement.
What is Form 1095-C?
Form 1095-C provides information about the health coverage provided by the employer. Applicable Large Employers (ALEs) must furnish Form 1095-C to their employees with information about their medical benefits for reporting purposes.
Choosing Form 1095-C Codes For Lines 14-16
Understanding how to select Form 1095-C codes for lines 14-16 can be challenging. Managing ACA compliance all year is demanding enough, but it's crucial to choose accurate codes for Forms 1095-C. Entering inaccurate codes can result in ACA penalties.
What Should You Include On Form 1095-C?
Here is what you should include on Form 1095-C for every employee:
- Line 14: What medical coverage did you offer your employee?
- Line 15: How much did the employee pay for the medical coverage offered?
- Line 16: What did the employee do when the offer was made, or why was it not made?
What Do The Codes On The ACA Form 1095-C Mean?
On line 14, the employer must indicate what type of coverage was provided to the employee for a specific tax year. Here are different codes that can be entered on line 14 of Form 1095-C:
- 1A
The 1A code indicates that a qualifying offer was made, and it complied with the requirements of the ACA's Employer Mandate. - 1B
This code communicates that the type of coverage provided met both Minimum Value (MV) and Minimum Essential Coverage (MEC) but was only provided to the employee and not to their dependents.
- 1C
This type of code indicates that MEC and MV health coverage was provided to the employee and their children but not to the spouse. - 1D
A 1D code indicates that MEC and MV health coverage was provided to the employee and the spouse but not their children. - 1E
The 1E code indicates that MEC and MV health coverage was offered to the employee, their children, and the spouse. - 1F
This code means that the coverage provided only met MEC and not MV. - 1G
A 1G code communicates that coverage was provided to an employee who was not full-time under the ACA. - 1H
The 1H code indicates that coverage was not offered or that coverage was offered, but it did not provide MEC.
Employers must also enter codes on line 16. Here are the different codes that can be entered on line 16 of Form 1095-C:
- 2A
The 2A code means that the employee was not employed. - 2B
This code indicates that the employee was not full-time. - 2C
A 2C code means that the employee enrolled in the coverage provided, regardless of whether or not the coverage complied with the ACA. - 2D
This code can be used if an employee is in a Limited Non-assessment Period and their ACA status has not been determined yet. - 2E
This type of code indicates multi-employer relief. - 2F
This code communicates that W-2 safe harbor was used to determine affordability for the employee.
- 2G
This code means that the Federal Poverty Line (FPL) safe harbor was used to prove that the coverage provided by the employer was affordable. - 2H
A 2H code indicates that the Rate of Pay safe harbor was used to prove that the coverage provided by the employer was affordable.
Takeaway
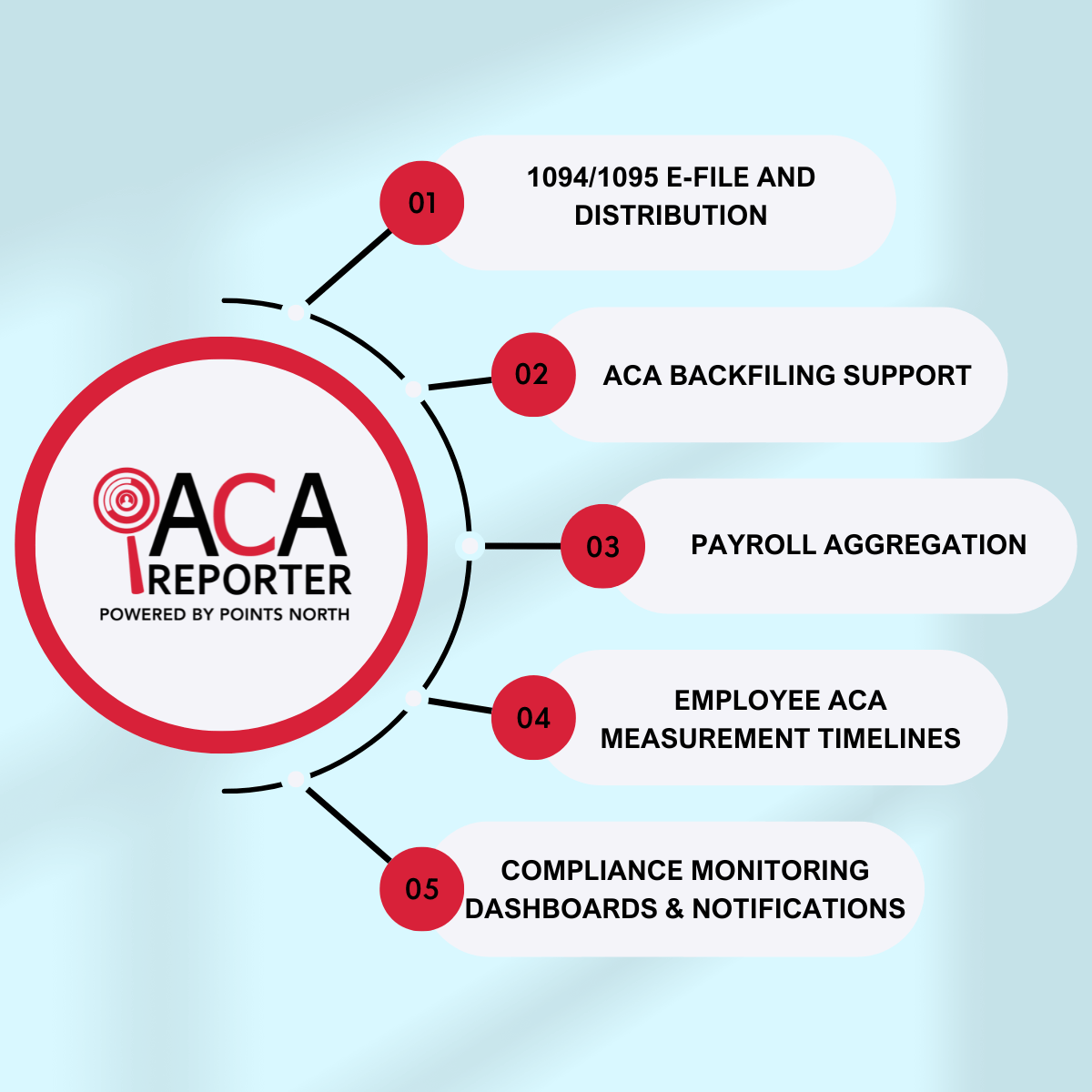
Employers who are unsure of how to code their ACA Form 1095-C should undergo an ACA Penalty Risk Assessment to determine their potential IRS penalty exposure. To learn more about how our ACA Reporter product can help keep you ACA compliant, contact us here!



.png)